Volume 11, Issue 30 of Oncotarget reported that previously, the authors showed that anti-estrogen drugs combined with a dendritic cell-based anti-HER-2 vaccine known to induce strong Th1-polarized immunity dramatically improved clinical response rates in patients with HER-2pos/ERpos early breast cancer.
Here, the Oncotarget authors show that the small molecule Akt antagonist MK-2206, when combined with the Th1 cytokines IFN-gamma and TNF-alpha, maximize indicators of apoptotic cell death in a panel of phenotypically-diverse human breast cancer lines.
These findings were mirrored by other, structurally-unrelated Akt-targeting drugs that work through different mechanisms. Interestingly, they found that MK-2206, as well as the other Akt antagonist drugs, also had a tendency to suppress Th1 cytokine expression in stimulated human and murine lymphocytes, potentially complicating their use in conjunction with active immunotherapy.
"They found that MK-2206, as well as the other Akt antagonist drugs, also had a tendency to suppress Th1 cytokine expression in stimulated human and murine lymphocytes, potentially complicating their use in conjunction with active immunotherapy"
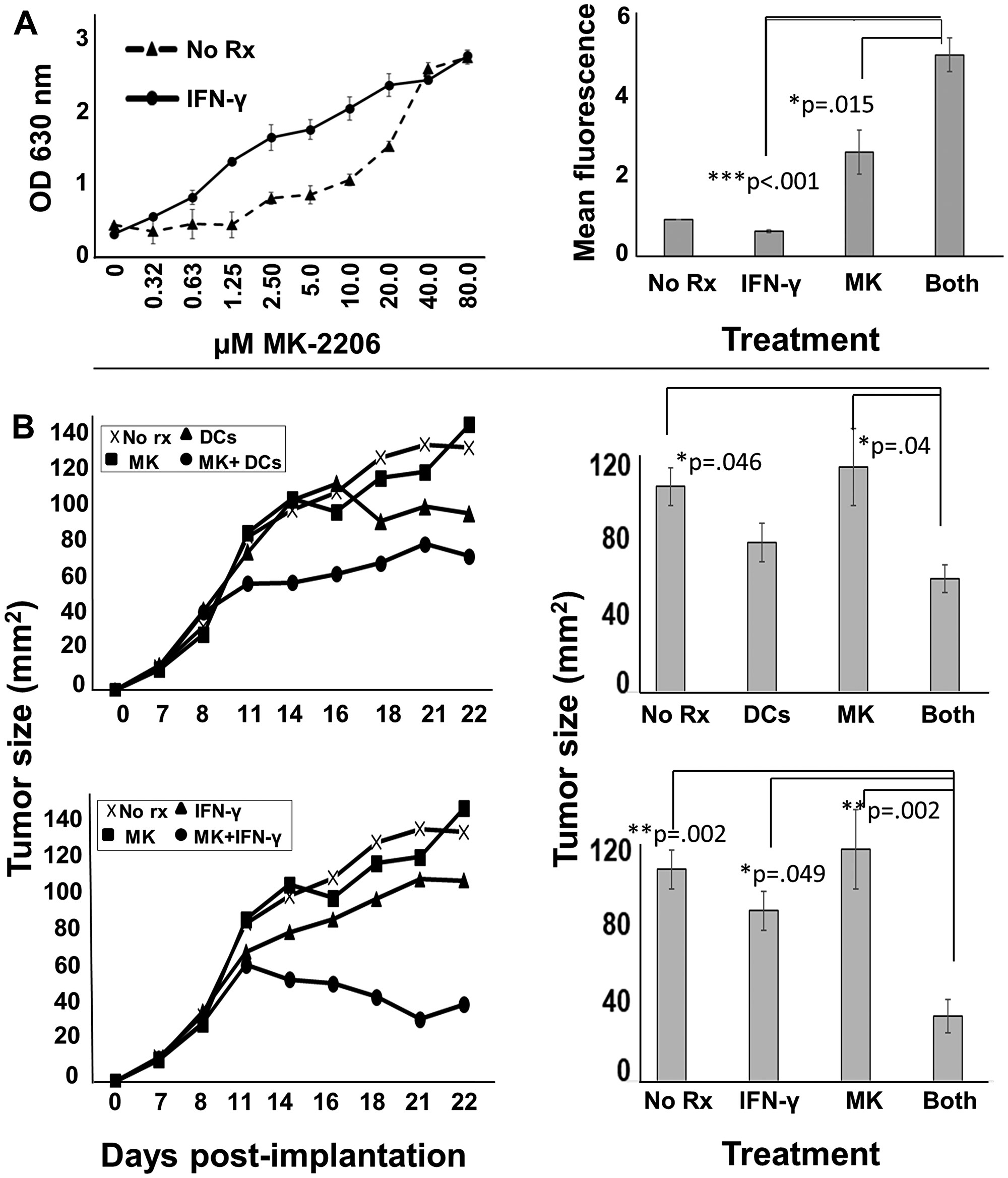
After verifying that MK-2206 plus IFN-gamma could show similar combined effects against breast cancer lines, even in the absence of TNF-alpha, the authors tested in a rodent HER-2pos breast cancer model either a HER-2-based DC vaccine, or recombinant IFN-gamma with or without MK-2206 administration.
These findings suggest a combined therapy approach for Akt-targeting drugs that incorporates recombinant Interferon-gamma and is potentially translatable to humans.
Dr. Gary K. Koski from Kent State University said "Once existing only at the margins of cancer treatment, immunotherapy has now gained a strong claim as a distinct and accepted treatment modality, taking its place among the established approaches of surgery, radiation, cytotoxic agents and targeted drugs."
Consistent with this notion, the authors and others have found that paired Th1 cytokines IFN-γ and TNF-α induced senescence and/or apoptosis in vitro for a variety of cancer cell lines.
Subsequent in vitro studies showed that ERpos BT-474 cells were relatively resistant to Th1 cytokines while ERneg SK-BR3 cells were more sensitive.
However, addition of anti-estrogen drugs to cytokines for BT-474 cells had about the same impact as cytokines alone on SKBR3, i. e. the drugs that blocked estrogen signaling appeared to sensitize estrogen-dependent cells to the Th1 cytokines.
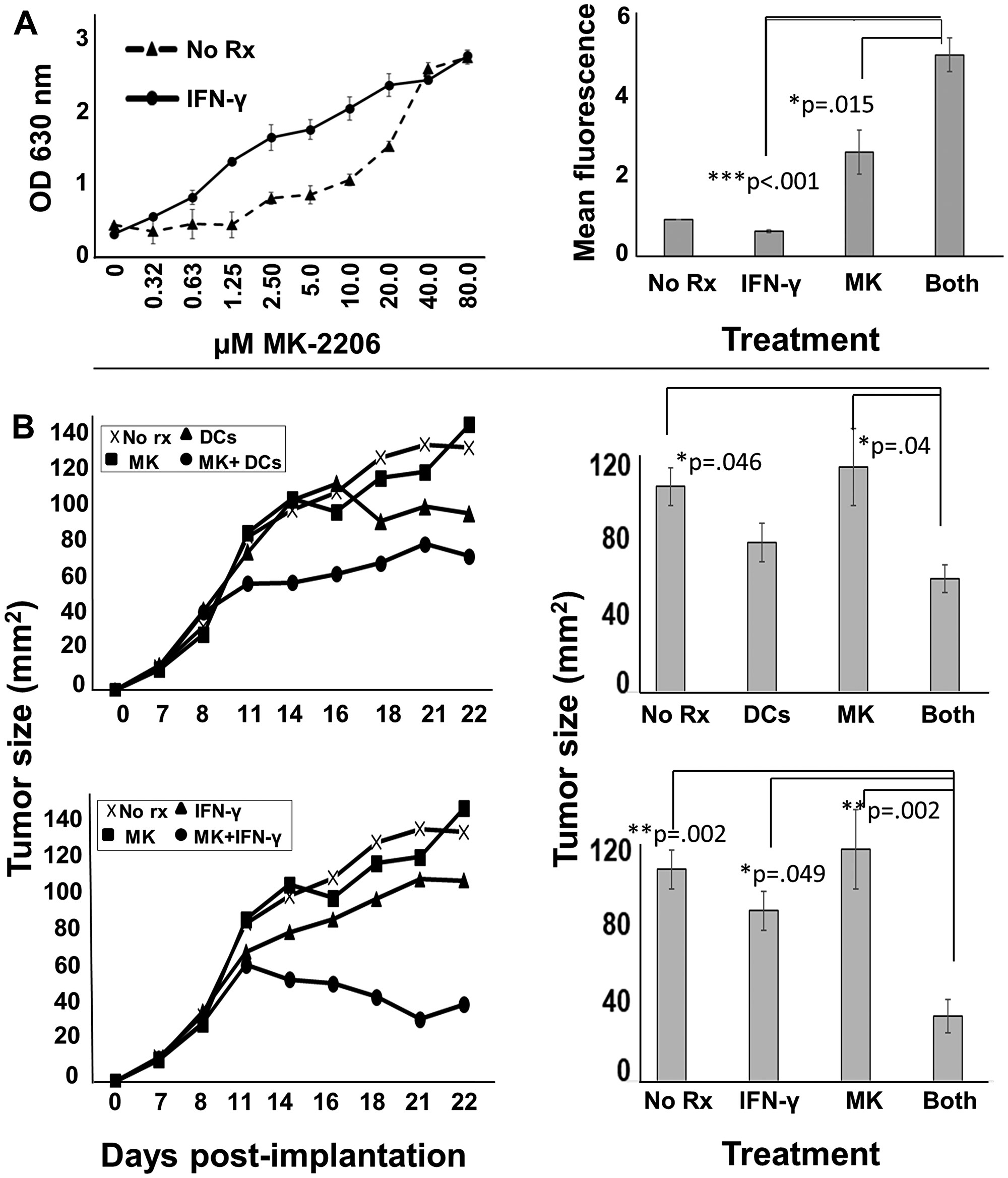
Figure 8: MK-2206 in conjunction with immunotherapy slows progression of rodent HER-2pos tumors. (A) Erbb2pos (rat homolog of HER-2) TUBO cells were cultured overnight in 96-well culture plates. The next day they were exposed to increasing concentrations of MK2206 in the presence (solid circles) or absence (dotted triangles) of IFN-γ (50 ng/ml) and incubated a further 72 h, after which 20 μl of resazurin sodium salt solution (1.4 mg/ml) was added to each well, and upon color change, optical density of culture supernatants assessed at 630 nm (left panel). Cells similarly treated were also assessed by Trypan Blue staining, and dye uptake evaluated by flow cytometry (right panel). Error bars indicate SEM. (B) 5 × 105 TUBO cells were implanted into the fat pad of one of the right mammary glands of female Balb/c mice. When tumors became palpable (seven days), mice were provided with six treatment regimens (5 mice per group) including no treatment (upper and lower panels), MK2206 (upper and lower panels), rat HER-2 peptide-pulsed dendritic cells (upper panels), peptide-pulsed DCs plus MK2206 (upper panels), IFN-γ (lower panels) and IFN-γ plus MK2206 (lower panel). MK2206 was supplied in two 5-day cycles separated by a 2 day rest period. IFN-γ was supplied on the same schedule as MK-2206. DCs were administered twice weekly during cycles of MK2206 treatment. Tumor growth was monitored 2–3 times per week. Growth curves are displayed in left panels, and statistical analysis at the terminus of treatment displayed in right panels. Error bars indicate SEM.
Because Akt sits at the nexus of such important growth and survival signaling pathways, and because we previously showed that Th1 cytokines also trigger apoptosis while lowering expression of HER family oncodriver expression, the authors hypothesized that the combination of Th1 cytokines and Akt antagonists might make a particularly effective pairing useful for immunotherapy of breast cancer.
Since MK-2206 is one of the most potent and best-studied Akt agonists, they designed a series of studies around this agent to determine whether a phenotypically diverse panel of breast cancer lines would be susceptible to combined action of Th1 cytokines and MK-2206, whether this combination would enhance cell death through an apoptotic mechanism, and determine the effect of this treatment on the expression of important oncodrivers by breast cancer cells.
The Koski Research Team concluded in their Oncotarget Research Paper that few studies have examined the impact of Akt antagonist drugs on T cell function.
In contrast, the authors focused their investigation on suppression on T cell function, namely the capacity of antigen- and mitogen-stimulated cells to produce IFN-γ.
They showed that MK-2206, as well as all other tested Akt antagonists, strongly suppressed IFN-γ production by stimulated lymphocytes.
It is entirely possible that one of the reasons Akt inhibitor drugs have underperformed expectations clinically is that they simultaneously suppress activated T cells, and particularly their capacity to produce cytokines like IFN-γ which might be critical for anti-tumor activity by the immune system.
In light of this developing clinical trial, in the present study the authors placed particular emphasis on trastuzumab- and lapatinib-resistant cell lines, positioning Akt antagonist drugs as possible ways to deal with resistance to these more established drugs, should they come to be used more routinely in conjunction with IFN-γ.
Sign up for free Altmetric alerts about this article
DOI - https://doi.org/10.18632/oncotarget.27556
Full text - https://www.oncotarget.com/article/27556/text/
Correspondence to - Gary K. Koski - [email protected]
Keywords - breast cancer, Akt kinase, immunotherapy
About Oncotarget
Oncotarget is a biweekly, peer-reviewed, open access biomedical journal covering research on all aspects of oncology.
To learn more about Oncotarget, please visit https://www.oncotarget.com or connect with:
SoundCloud - https://soundcloud.com/oncotarget
Facebook - https://www.facebook.com/Oncotarget/
Twitter - https://twitter.com/oncotarget
LinkedIn - https://www.linkedin.com/company/oncotarget
Pinterest - https://www.pinterest.com/oncotarget/
Reddit - https://www.reddit.com/user/Oncotarget/
Oncotarget is published by Impact Journals, LLC please visit http://www.ImpactJournals.com or connect with @ImpactJrnls
Media Contact
[email protected]
18009220957x105