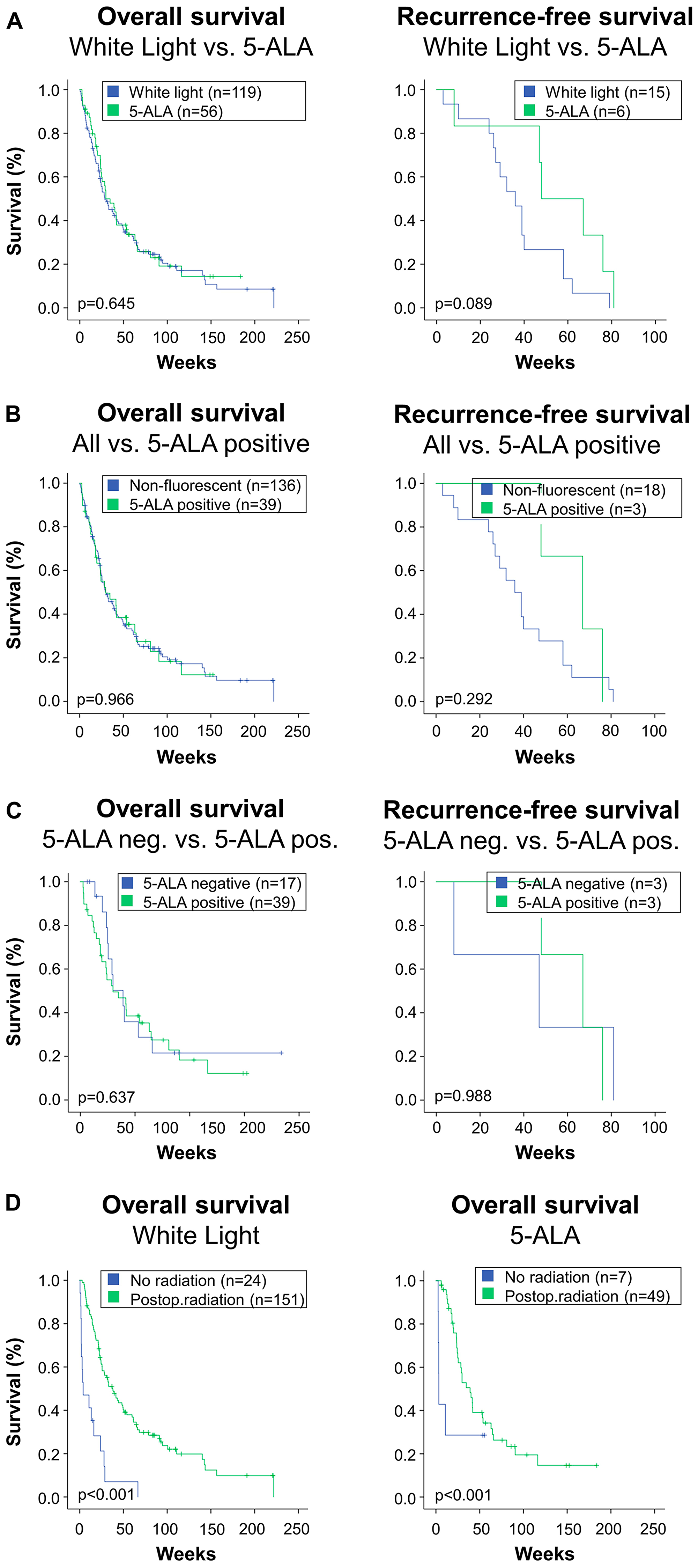
The cover for issue 32 of Oncotarget features Figure 2, "This figure depicts overall survival and local in-brain recurrence-free survival in the study's subgroups," by Hussein, et al. which reported that the aim of the present study is to assess whether the use of 5-ALA has an impact on local recurrence or survival compared to conventional white light microscopic tumor resection.
Two groups were compared:
In the “white light” group, resection was performed with conventional microscopy.
In the 5-ALA group, fluorescence guided peritumoral resection was additionally performed after standard microscopic resection.
Local in-brain recurrence occurred in 21/175 patients with a rate of 15/119 in the white light and 6/56 in the 5-ALA group.
The use of 5-ALA did not result in lower in-brain recurrence or mortality compared to the use of white light microscopy.
Dr. Bawarjan Schatlo from the Department of Neurosurgery at The University of Medicine Goettingen said, "Metastatic brain disease is more common than primary brain tumors."
"Metastatic brain disease is more common than primary brain tumors."
Another group made the case for extending tumor resection 5 millimeters into peritumoral tissue to perform a so-called supramarginal resection.
Its aim is to prolong progression-free survival through radical resection and improved local tumor control.
In a series of 52 patients, Kamp and colleagues detected positive fluorescence in 62% of resected cerebral metastases.
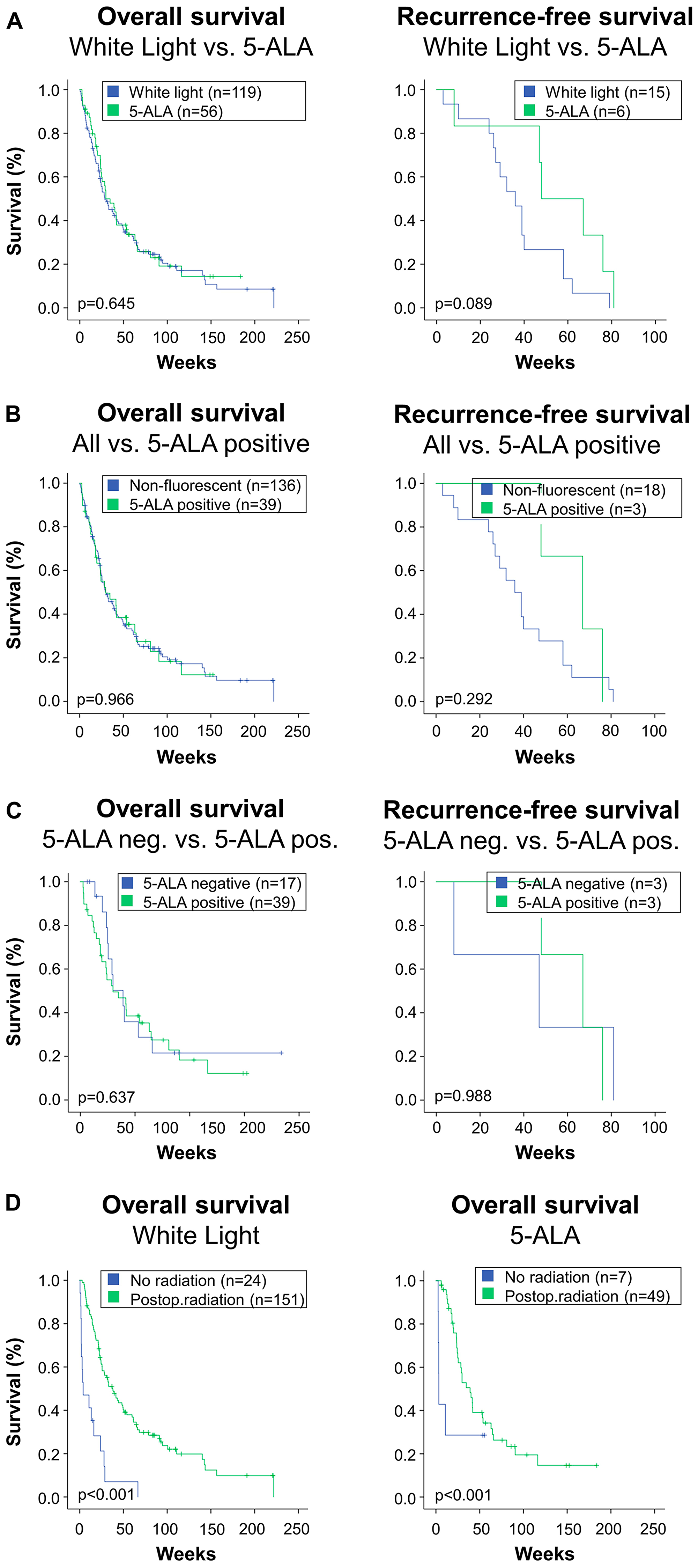
Figure 2: This figure depicts overall survival and local in-brain recurrence-free survival in the study's subgroups. : This figure depicts overall survival and local in-brain recurrence-free survival in the study's subgroups. (A) Patients who were operated under microscopic white light were compared to patients who received 5-ALA. The 5-ALA group comprises all patients receiving the fluorescent dye, irrespective of the actual intraoperative finding of fluorescence. Log rank comparison showed no difference in overall survival (left), while there was a trend towards higher recurrence-free survival in the 5-ALA group (right). (B) About one third of patients who received 5-ALA did not exhibit fluorescence during surgery. Therefore, although they were attributed to the 5-ALA group in the analysis, the surgeon was not able to use fluorescence. Therefore, an “as treated” analysis was performed. Therein, all patients who were 5-ALA negative, i. e. received 5-ALA but showed no fluorescence intraoperatively, were added to the White Light-group. This results in a 5-ALA positive versus “all others” or “non-fluorescent” comparison. This analysis revealed no difference in overall or recurrence-free survival between groups in the Kaplan log rank comparisons. (C) For a subgroup analysis, patients who received 5-ALA were split in two groups. The first one represents the lack of intraoperative fluorescence (5-ALA neg.), and the other includes patients where red fluorescence was visible (5-ALA pos.). This subgroup analysis revealed no inter-group differences in overall or recurrence-free survival. (D) Radiotherapy significantly impacts survival. For internal data validation purposes, the impact of radiotherapy was compared in the study's main groups: White light microscopy (left) versus patients who received 5-ALA (right). In both groups, the marked effect of radiotherapy was reconfirmed.
Thus, the utility and importance of using methods to improve local control of brain metastases remains an unresolved issue.
The aim of the current study was to compare survival and local recurrence in a cohort of patients who underwent surgery for brain metastases with 5-ALA fluorescence microscopy to one that was operated using microscopic white light only.
The Schatlo Research Team concluded in their Oncotarget Research Paper, "the present study confirmed that regardless of surgical adjunct, radiotherapy is strongly associated with improved survival."
Sign up for free Altmetric alerts about this article
DOI - https://doi.org/10.18632/oncotarget.27688
Full text - https://www.oncotarget.com/article/27688/text/
Correspondence to - Bawarjan Schatlo - [email protected]
Keywords - brain tumor, brain metastasis, fluorescence-guided surgery, 5-ALA
About Oncotarget
Oncotarget is a biweekly, peer-reviewed, open access biomedical journal covering research on all aspects of oncology.
To learn more about Oncotarget, please visit https://www.oncotarget.com or connect with:
SoundCloud - https://soundcloud.com/oncotarget
Facebook - https://www.facebook.com/Oncotarget/
Twitter - https://twitter.com/oncotarget
LinkedIn - https://www.linkedin.com/company/oncotarget
Pinterest - https://www.pinterest.com/oncotarget/
Reddit - https://www.reddit.com/user/Oncotarget/
Oncotarget is published by Impact Journals, LLC please visit http://www.ImpactJournals.com or connect with @ImpactJrnls
Media Contact
[email protected]
18009220957x105