The researchers have recently identified the tumor suppressor tuberous sclerosis complex 1 as a new co-chaperone of Hsp90 that affects Hsp90 binding to its inhibitors.
Their findings suggest that TSC1 status may predict response to Hsp90 inhibitors in patients with bladder cancer, and co-targeting HDACs can sensitize tumors with Tsc1 mutations to Hsp90 inhibitors.
Dr. Mehdi Mollapour and Dr. Dimitra Bourboulia said, "Over 80,000 people will be diagnosed with bladder cancer and approximately 18,000 patients will die from this disease in the United States in 2019."
Additionally, Tsc1 assists in the deceleration of Hsp90 ATPase activity and the Hsp90 chaperone cycle, and Tsc1 expression increases Hsp90 binding to its inhibitors.
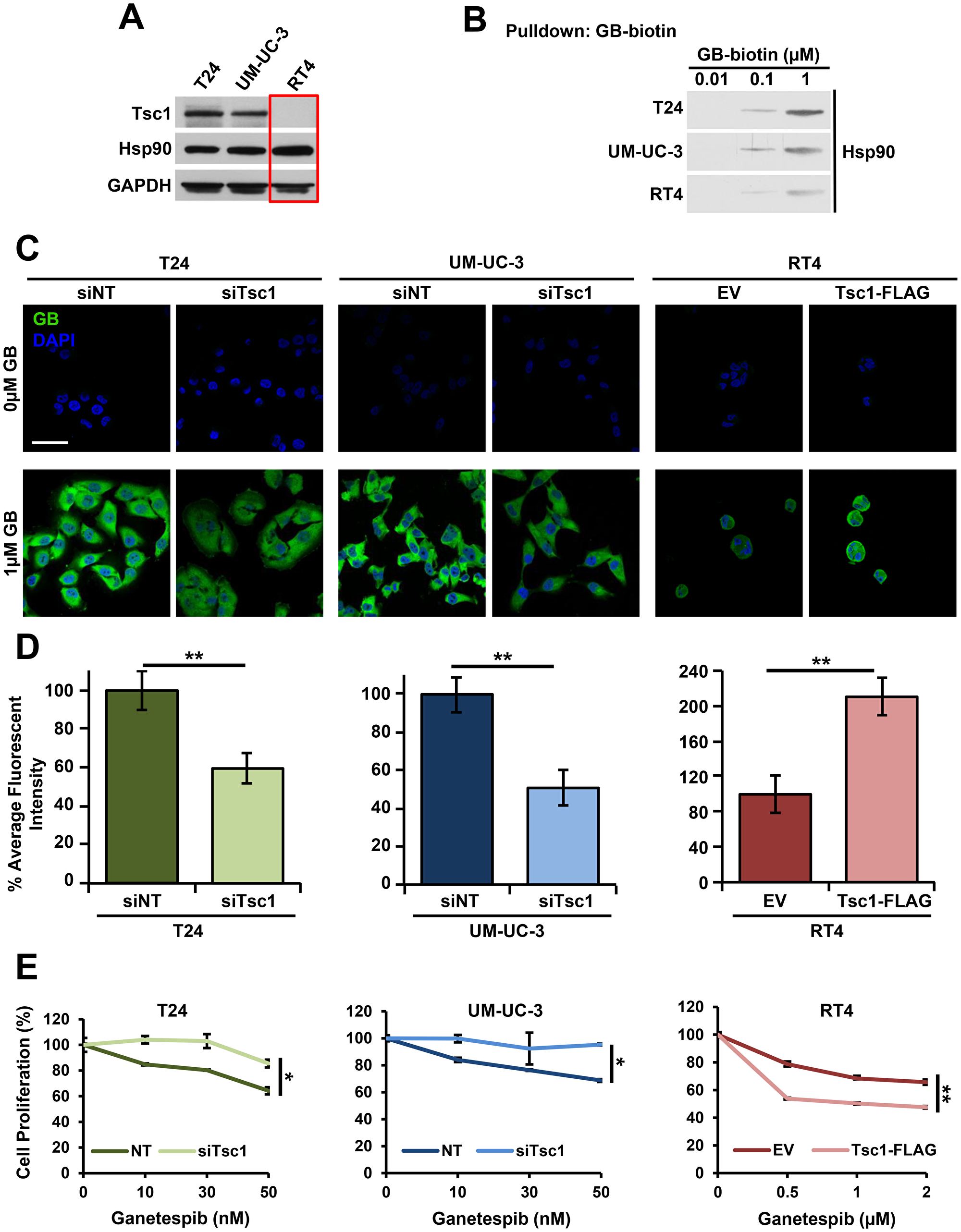
Figure 1: Tsc1 expression determines Hsp90 inhibitor accumulation and sensitivity in bladder cancer cells. (A) Tsc1 status in T24, UM-UC-3 and RT4 bladder cancer cell lines was assessed by immunoblot. GAPDH was used as a loading control. (B) Lysates from Figure 1A were challenged with biotinylated-ganetespib. Binding of Hsp90 from T24, UM-UC-3 and RT4 cells to biotinylated-ganetespib was examined by immunoblot. (C) TSC1 was targeted by siRNA in T24 and UM-UC-3 cells and Tsc1-FLAG was transiently expressed in RT4 cells. Representative confocal microscopy images of these cells treated for 4hr with BODIPY-ganetespib at the indicated concentrations and stained with DAPI. Scale bar = 50 μm. (D) Quantification of average fluorescence intensity of BODIPY-ganetespib in (C). A Student's t-test was performed to assess statistical significance (**p < 0.01). (E) TSC1 was targeted by siRNA in T24 (left) and UM-UC-3 (center) and Tsc1-FLAG was transiently expressed in RT4 (right) cells for 48 hr. Following this, cells were treated for an additional 72 hr with the indicated concentrations of ganetespib. Cell proliferation was assessed by WST proliferation assay. A Student's t-test was performed to assess statistical significance (*p < 0.05; **p < 0.01).
Mutation and inactivation of the tumor suppressor TSC1 has been found in approximately 15% of bladder cancers and loss of heterozygosity of a region spanning the TSC1 locus at 9q34 has been seen in roughly 54% of bladder cancers.
The authors therefore hypothesized that mutation and inactivation of TSC1 in bladder cancer cells leads to decreased sensitivity to Hsp90 inhibitors.
Their data supported this hypothesis, and they mechanistically demonstrated that mutation and loss of TSC1 in bladder cancer cells causes hypoacetylation of Hsp90-K407/K419 and subsequent decreased binding of Hsp90 to its inhibitor ganetespib.
Their results suggest that Tsc1 status can predict response to Hsp90 inhibition in bladder cancer patients and further provide a strategy to co-target HDACs and Hsp90 in bladder cancers with mutation in TSC1.
The Mollapour/Bourboulia Research Team concluded that this research suggests that TSC1 status may predict sensitivity to Hsp90 inhibitors in bladder cancer.
Additionally, in those patients with TSC1 mutated bladder cancer, inhibition of HDACs can potentially restore Hsp90 acetylation and sensitivity to Hsp90 inhibitors. HDAC6 mediated deacetylation of Hsp90 and regulation of its chaperone function has been reported previously.
Full text - https://doi.org/10.18632/oncotarget.27217
Correspondence to - Melanie Haas Kucherlapati - [email protected] and Dimitra Bourboulia - [email protected]
Keywords - tuberous sclerosis complex (TSC), Tsc1 (Hamartin), Tsc2 (Tuberin), heat shock protein (Hsp90), bladder cancer