Patients with limited treatment options have poor survival and may die from painful local and systemic disease progression.
However, stereotactic body radiation therapy is a promising, minimally invasive treatment that can result in local control, symptom palliation, and possibly extended survival outcomes as a primary treatment with an acceptable toxicity profile with similar survival and toxicity outcomes when delivered with both Cyberknife and linear accelerator-based approaches.
Two small retrospective studies have reported that SBRT may be a feasible and safe treatment for elderly patients with medical comorbidities and may provide relief of abdominal pain in as many as 79% of patients.
The research team said that "While this study demonstrates SBRT is a viable treatment option even in the setting of severe comorbidities, poor performance status, and advanced age, future studies are warranted to further elucidate the importance of chemotherapy in relation to SBRT and to assess the impact of SBRT on patient reported measures of quality of life."
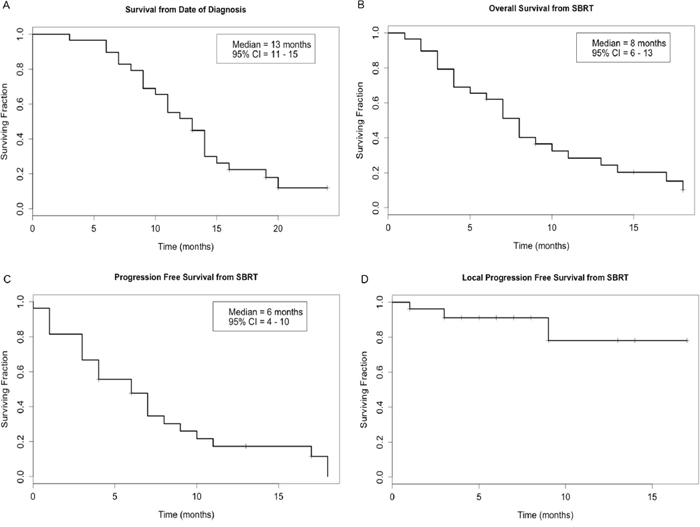
Figure 1: Kaplan-Meier curves showing (A) survival from the date of histologic diagnosis and (B) overall survival, (C) progression-free survival, and (D) local progression-free survival from the date of the first fraction of stereotactic body radiation therapy (SBRT). CI indicates confidence interval.
While most clinical trials for localized PDAC focus on patients who can tolerate aggressive multi-modality therapy including surgery, chemotherapy, and/or radiation, it is important to find treatment options for patients who cannot tolerate existing therapies, especially considering the prevalence of debilitating symptoms associated with PDAC and comorbid conditions in elderly patients.
SBRT is a promising local therapy that has been studied as an alternative to conventionally fractionated radiation therapy. Compared the outcomes of 7,819 patients treated with conventionally fractionated radiation therapy to 631 patients treated with SBRT.
In a study of 44 patients treated with SBRT and 226 patients treated with intensity modulated radiation therapy, SBRT was associated with lower rates of grade 2 and 3 acute toxicities than IMRT, although no difference in OS was found.
In addition to possibly improved survival and lower rates of toxicity, SBRT can be delivered in only 5 fractions, while conventionally fractionated radiation therapy can take more than 20 days.
With low rates of toxicity and encouraging local disease control, SBRT could be preferred over palliative chemotherapy alone or best supportive care in patients with localized disease who cannot undergo surgical resection.
In addition, 22 patients in their study received induction chemotherapy before SBRT and only 5 patients did not receive any chemotherapy before or after SBRT. Only 4 patients received induction chemotherapy, 6 patients received maintenance chemotherapy, and 16 did not receive any chemotherapy.
In the study by Yechieli et al., no patients received chemotherapy before SBRT, and only one received maintenance capecitabine after SBRT.
In fact, in their study patients receiving induction chemotherapy prior to SBRT had superior survival outcomes than patients who did not receive induction chemotherapy before SBRT.
In the current study, patients experienced high rates of symptom palliation after receiving SBRT, especially patients who experienced abdominal pain and nausea prior to the start of treatment.
The capacity of SBRT to improve patient's symptoms and the relatively short period of SBRT delivery make this treatment modality an especially attractive option for patients prioritizing quality of life.
The outcomes of patients with localized PDAC who were treated with SBRT at the research institution after being deemed medically inoperable due to advanced age, medical comorbidities, and/or poor performance status.
Full text - https://doi.org/10.18632/oncotarget.24713
Correspondence to - Joseph M. Herman - [email protected]
Keywords - stereotactic body radiation therapy (SBRT), palliative care, pancreatic cancer, radiation, elderly